Amputation Prevention
Symptoms
More than 80 percent of amputations begin with foot ulcers due to poor circulation in legs. A non-healing ulcer that causes severe damage to tissues and bone may require surgical removal (amputation) of a toe, foot or part of a leg.
There are many reasons why chronic wounds don’t heal but the primary reason is due to the poor circulation in legs or even bad circulation in foot. The good news is that we can improve circulation in your legs and decrease your chances of amputation if your condition is addressed and treated in a timely manner by a vascular specialist doctor.
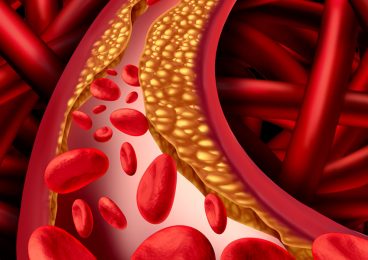
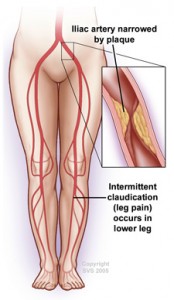
Let’s learn more about poor circulation, why it happens and what is does to the body. People with poor circulation – for instance, as a result of peripheral artery disease (P.A.D.) – have arteries that are narrowed by plaque buildup which obstructs normal blood flow. Healthy arteries are smooth and unobstructed, allowing blood to flow freely throughout the body. This is especially important for people with diabetes or peripheral artery disease.
Who is at Risk?
Here are some causes and risk factors of poor circulation that prevent the healing process in wounds.
- Age
- High blood pressure
- Diabetes
- Smoking
- High cholesterol
- Obesity
- Lack of exercise
- Family history of vascular problems.
When you have one or more of these factors you increase your risk of having plaque, which is a sticky substance made up of fat and cholesterol that builds up in the arteries. This buildup of plaque causes the passageway in the arteries to become narrow which in turn limits the blood flow to your extremities. If left untreated, this will cause non-healing sores, wounds, foot ulcers or infections which can lead to amputations, heart attack or stroke.
Symptoms
Early detection is key to avoid serious complications, so keep an eye out for the following symptoms, especially in the lower extremities such as legs and feet:
- Non-healing sores
- Chronic wounds
- Foot ulcers
- Infections
The good news is if the root cause of poor circulation is treated quickly, the symptoms can be reversed.
What Tests are Needed?

Ankle-Brachial Index (ABI)
You may be given an Ankle-Brachial Index (ABI) test to compare the blood pressure in your ankle and your arm, which are normally the same. If the blood pressure in your ankle is significantly lower, that could be a sign of narrowing leg arteries.
Doppler Ultrasound
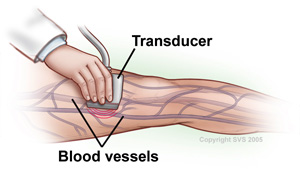
Ultrasound may be used to determine which arteries are blocked. Often, angiography is used to find the specific location and pattern of any blockages. Angiography helps specifically identify the best way to correct aortoiliac disease. Both MRA and CTA are also helpful in outlining the extent of aortoiliac disease.
Testing can be done in the PVA Vascular Lab.
Treatments
The first step is to see a doctor vascular surgery immediately if you have any of the risk factors or symptoms listed above. A simple, painless and noninvasive test called a duplex ultrasound can determine if you have poor circulation and the severity of the condition.
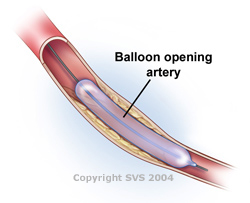
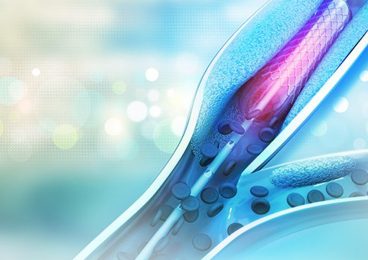
Based on the severity of your condition, a vascular specialist doctor will determine the best treatment option for you. This may include lifestyle changes, medications, minimally invasive cath lab procedures such as angioplasty or stenting, which can be done in a PVA office, or open bypass surgery.
At PVA, we are blood circulation experts. Each and every day, we focus our knowledge and expertise on improving circulation in feet and throughout the body to help our patients avoid amputation. Vascular surgeons are the only doctors treating blood circulation problems today who can perform all treatment options available including medical management, minimally invasive procedures and open surgical repair including bypass.
Only when you see a vascular expert who offers all treatment options, can you be assured of receiving the care that is most appropriate to improve circulation and prevent further wounds from developing.