Thoracic Aneurysms
An aneurysm occurs when the walls of the aorta become weak and the diameter of the aorta increases.
The thoracic aorta is the part of your aorta that runs through your chest. A thoracic aortic aneurysm (TAA) occurs when a weak area of your thoracic aorta expands or bulges. Approximately 25 percent of aortic aneurysms occur in the chest, and the rest involve the abdominal aorta.
Thoracic aortic aneurysms are serious health risks because they can burst or rupture. A ruptured aneurysm can cause severe internal bleeding, which can rapidly lead to shock or death.
Who is at Risk?
Risk factors include smoking, high blood pressure, and having a family history of aneurysms.
In addition, an aortic dissection, typically associated with high blood pressure, may cause an aortic aneurysm to develop. An aortic dissection occurs when blood flow forces the layers of the wall of your aorta apart, which weakens your aorta.
Certain other diseases can weaken the layers of the aortic wall, increasing the risk of aneurysms. These diseases include:
- Marfan’s syndrome, a connective tissue disorder
- Syphilis
- Tuberculosis
Your risk of developing TAA increases as you age. TAA is more common in men than in women. The larger your TAA, or the faster it grows, the more likely it is to rupture. The chance of rupture increases when your aneurysm is larger than about twice the normal diameter.
Symptoms
Symptoms of an aortic dissection include chest and/or back pain. It can often mimic the symptoms of a heart attack. If you experience chest or back pain, you should notify your physician immediately.
Tests and Treatments
Your physician will order one or more of the following tests to diagnose TAA:
- Chest x-ray
- Echocardiography (an ultrasound of the heart)
- Magnetic resonance imaging (MRI)
- Computed tomography (CT) scan
- Angiography
If your TAA is small and not causing symptoms, your physician may recommend “watchful waiting,” which means that you will be monitored every 6 months for signs of changes in your aneurysm
However, if your TAA is large or causing symptoms, you need active and prompt treatment to prevent rupture. Your vascular surgeon may recommend actively treating your aneurysm if it is large, grows quickly, or you have certain other types of disease. For example, if you have Marfan’s syndrome, you may require active treatment sooner than patients who have small TAAs but do not have Marfan’s syndrome. The active treatments for TAA are open surgical aneurysm repair and endovascular stent-graft repair.
Testing can be done in the PVA Vascular Lab.
Open Surgical Repair
During open aneurysm repair, your surgeon makes an incision in your chest and replaces the weakened portion of your aorta with a fabric tube, called a graft. The graft is stronger than the weakened aorta and allows blood to pass through it without causing a bulge. Many patients who have a TAA also have heart disease or involvement of the aorta adjacent to the heart. Extensive or complex thoracic aneurysms may require heart surgery at the same time as open aneurysm repair.
Following the surgery, you may stay in the hospital for 7 to 10 days. If your aneurysm is extensive or complex, or if you have other conditions such as heart, lung or kidney disease, you may require 2 to 3 months for a complete recovery.
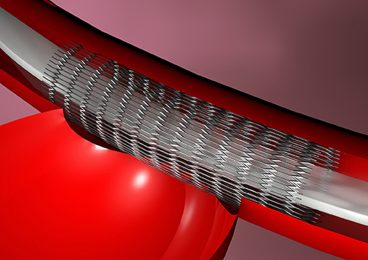
Endovascular Stent Graft Repair
Instead of open aneurysm repair, if your aneurysm location and shape is suitable, your vascular surgeon may consider a promising, newer procedure called an endovascular stent graft. Endovascular means using long, thin tubes called catheters inside your body to perform the treatment. The catheters are inserted in small incisions in your groin, and sometimes your arms, and are guided through your blood vessels.
During the procedure, your surgeon will use live x-ray pictures viewed on a video screen to guide a stent-graft to the site of your aneurysm. Like the graft used in open surgery, this stent-graft allows blood to flow through your aorta without putting pressure on the damaged wall of your aneurysm. This keeps your aneurysm from rupturing.
Over time, your aneurysm usually will shrink. Endovascular stent-graft repair requires a shorter recovery time than open aneurysm repair, and your hospital stay is reduced to 2 of 3 days. However, this treatment may not be applicable to all TAAs, since your aneurysm must have a suitable shape to allow the stent-graft to be used effectively.
With the endovascular stent-graft repair, it is particularly important that long-term follow-up with periodic scans of the aortic repair be done to be sure that the stent-graft is functioning properly. Sometimes further procedures are required to maintain the stent-graft if leaks develop or if it moves out of position. Experts are still studying the long-term results of endovascular stent-graft repair.
Your vascular surgeon will advise you regarding the best option for your particular situation.
http://www.vascularweb.org/vascularhealth/Pages/thoracic-aortic-aneurysm.aspx