Carotid Stent
What is carotid artery stenting?
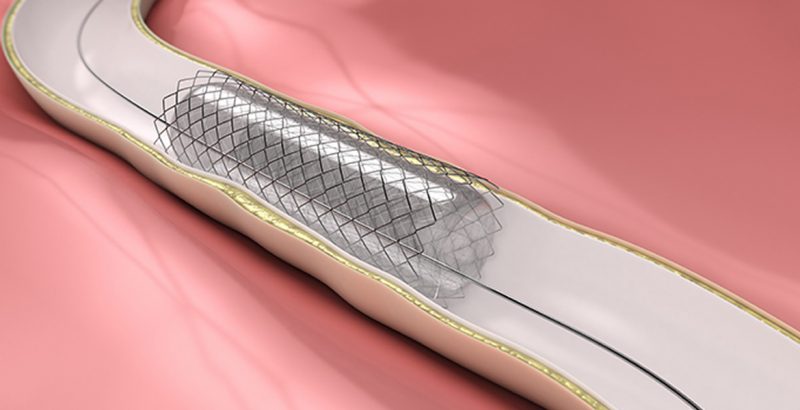
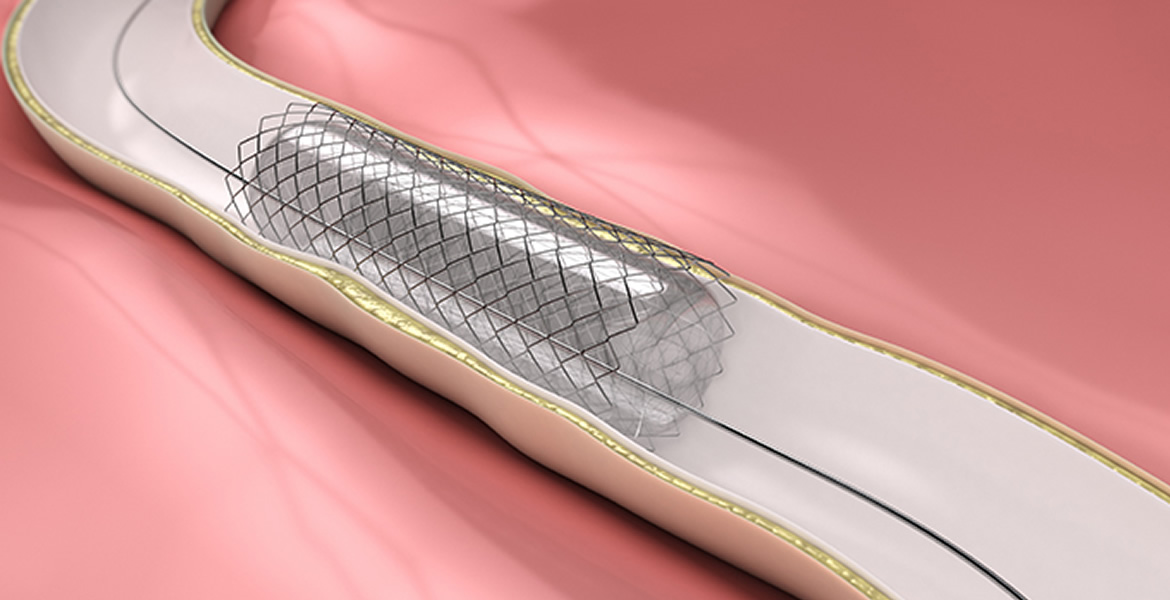
Carotid artery stenting is a procedure in which your vascular surgeon inserts a slender, metal-mesh tube, called a stent, which expands inside your carotid artery to increase blood flow in areas blocked by plaque. Hardening of the arteries, also known as atherosclerosis, can cause a build-up of plaque. In hardening of the arteries, plaque builds up in the walls of your arteries as you age. Cholesterol, calcium, and fibrous tissue make up the plaque. As more plaque accumulates, your arteries can narrow and stiffen. Eventually, enough plaque may build up to reduce blood flow through your arteries, or cause blood clots or pieces of plaque to break free and to block the arteries in the brain beyond the plaque.
Your carotid arteries are located on each side of your neck and extend from your aorta in your chest to the base of your skull. These arteries supply blood to your brain. You have one main carotid artery on each side, and each of these divides into two major branches, the external and the internal carotid arteries. The external carotid supplies blood to your face and scalp. Your internal carotid artery is more important because it supplies blood to the brain.
When plaque builds up and reduces blood flow in your carotid arteries, you have carotid artery disease. This is a serious issue because clots can form on the plaque and block the blood flow to your brain. If a clot or plaque blocks the blood flow to your brain, it can cause an ischemic stroke, which can cause brain damage or death. An ischemic stroke is a stroke that occurs because there is a lack of blood flow to cells in the brain. Another related problem that the plaque can cause is an arterial embolism. This occurs when a small piece of plaque or a blood clot breaks away from the site where it formed and blocks another artery downstream. If a clot blocks a tiny artery in the brain, it may cause temporary neurological symptoms, called transient ischemic attacks (TIAs), sometimes called “mini-strokes.”
When your physician wants to treat a blocked carotid artery, he or she, in some circumstances, may recommend that you have a stent inserted as an alternative to surgical removal of the plaque, known as carotid endarterectomy. During the carotid stenting procedure, your physician inserts a stent into your carotid artery after performing angioplasty. Angioplasty uses a balloon inflated in the narrowed part of the artery to flatten the plaque and open the artery. The stent holds the artery open by holding back the flattened plaque like scaffolding in a mineshaft.
How do I prepare?
Your physician may give you specific instructions to follow before the procedure, such as fasting. You should always inform your physician about any medications that you are taking.
In most cases, your physician will instruct you take aspirin and a prescription medication that prevents clots for 3 to 5 days before the procedure. Your physician may also order a duplex ultrasound, a computed tomography (CT) scan, an angiogram, or magnetic resonance imaging (MRI) to evaluate the degree of blockage in your carotid artery.
Am I a candidate for carotid stenting?
At the present time, carotid stenting has been approved for the treatment of patients with symptomatic carotid artery disease who are considered to be too high risk for carotid endarterectomy. You may be a candidate for the procedure if you are considered high risk for carotid endarterectomy, if your carotid artery is significantly narrowed (usually by more than 70 percent), and if you have had symptoms of a mini-stroke or stroke. If you fall outside of these categories, you may be a candidate for enrollment in a clinical trial evaluating the outcomes of carotid artery stent placement.
You may not be a candidate if you have one or more of the following:
- A life expectancy shorter than 2 years
- An irregular heart rhythm
- An allergy to any of the medications used in the procedure
- Bleeding in your brain within the last 2 months
- Complete obstruction of the carotid artery
Am I at risk for complications during carotid stenting?
Factors that may increase your chance for having complications during carotid stenting include:
- High blood pressure
- An allergy to contrast dye
- Hardened (calcified) and long narrowing of the carotid artery
- Sharp bends or other difficult anatomies in the carotid arteries
- Irregular-looking plaque
- Significant plaque or atherosclerosis of the aorta near the beginning of the carotid artery
- An age more than 80 years
- Extensive blockages in the arm and leg arteries
- Poor kidney function
What happens during carotid stenting?
The procedure usually takes place in an angiography suite or
catheterization lab. Before the procedure begins, your physician will connect you to a monitor that shows your heart rate and blood pressure. During the procedure, your physician will likely talk with you and may instruct you to squeeze a small toy or ball so that he or she can monitor your brain function. While some physicians may perform the procedure under general anesthesia, in most instances, the procedure is performed while you are awake and alert.
Your physician will give you medications such as heparin to prevent clots, atropine to reduce the chances of your heart slowing down, and a local anesthetic to numb the catheter insertion area. Your physician may not give you any other medications so you will be alert to follow instructions during the procedure. Your physician then locates the narrow areas in your arteries by injecting a dye into your arteries and taking live x rays, called fluoroscopy. The dye does not allow x rays to pass through, so physicians can see your arteries and use the live x rays to guide them to the blockage.
Before inserting the stent, your physician will usually perform angioplasty. In angioplasty, your physician inserts a long, thin tube called a catheter with an attached balloon into a small incision or puncture over an artery in your arm or groin. Your physician guides the catheter to the blockage site in your carotid artery using live x ray imaging. You will not feel the catheters as they move through your arteries because there are no nerve endings inside your arteries.
At this point in the procedure, your physician may insert a small balloon, basket, or filter called an embolic protection device. This device helps to prevent strokes by catching the clots or debris that may break away from the plaque during the procedure.
At the blockage site, your physician inflates and deflates the angioplasty balloon to flatten the plaque and widen the space where the blood flows through. After the artery is open, your physician then removes the catheter with the balloon attached.
Using another catheter, your physician guides a compressed stent to the same area in your carotid artery. Once the stent is in place, your physician releases it. The stent then expands to fit the artery. In most cases, your physician then uses a balloon catheter to further expand the stent.
Your physician then removes the stent-carrying catheter and any embolic protection devices. Stents remain permanently in your carotid artery. Because stents are made of stainless steel or metal alloys, they resist rust.
Carotid stenting usually takes about 1-2 hours but may take longer in some circumstances.
What can I expect after carotid stenting?
Immediately after the procedure, your physician applies pressure to the catheter insertion site in the groin or arm for 15 to 30 minutes to allow it to close and prevent bleeding. Sometimes to close the incision, your physician may use, instead, a cork-like closure device or stitches that dissolve.
If your physician inserts the catheters and other instruments through your femoral artery, your physician may instruct you to stay in bed for the next several hours so that he or she can watch for any complications, such as bleeding from the puncture site.
Your physician may instruct you not to lift anything more than about 5 to 10 pounds after you return home, to avoid any pressure on the incision. Your physician may also instruct you not to take a bath for a few days (but showers are usually fine), and to drink plenty of water to help flush the dye out of your system. You will be advised to take blood thinning medications and also be scheduled for periodic follow-up examinations, usually including carotid ultrasound examinations, to monitor the function of your stent over time.
Are there any complications?
Blockage by a clot or other debris in an artery in your brain, called an embolism, is the most serious complication that can occur after carotid stenting. This blockage can cause a stroke. Other complications that may cause a stroke include a blood clot forming along the stent or a tear in the artery wall called a dissection. The re-blockage of the carotid artery, called restenosis, is another possible complication. The dye used for the angiogram can sometimes cause damage to the kidneys, especially in people who already have kidney trouble. Bleeding from the puncture site in the groin or arm artery, called a hematoma or a false aneurysm, can also occur, but this is unusual. Bruising and mild tenderness at the puncture site is common, however, and usually resolves with time.
What can I do to stay healthy?
Although carotid stenting opens your artery and keeps blood flowing, it does not stop plaque from building up. To prevent hardening of the arteries from occurring again, you should consider the following changes:
- Eat more foods low in saturated fat, cholesterol, and calories
- Exercise regularly, especially aerobic exercises such as walking
- Maintain your ideal body weight
- Quit smoking
- Follow your physician’s recommendations for medications to control cholesterol and to thin the blood