Aneurysm Repair
What is an endovascular stent graft?
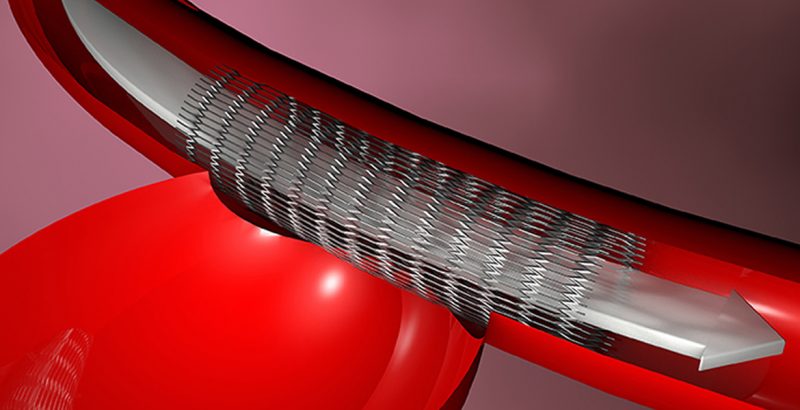
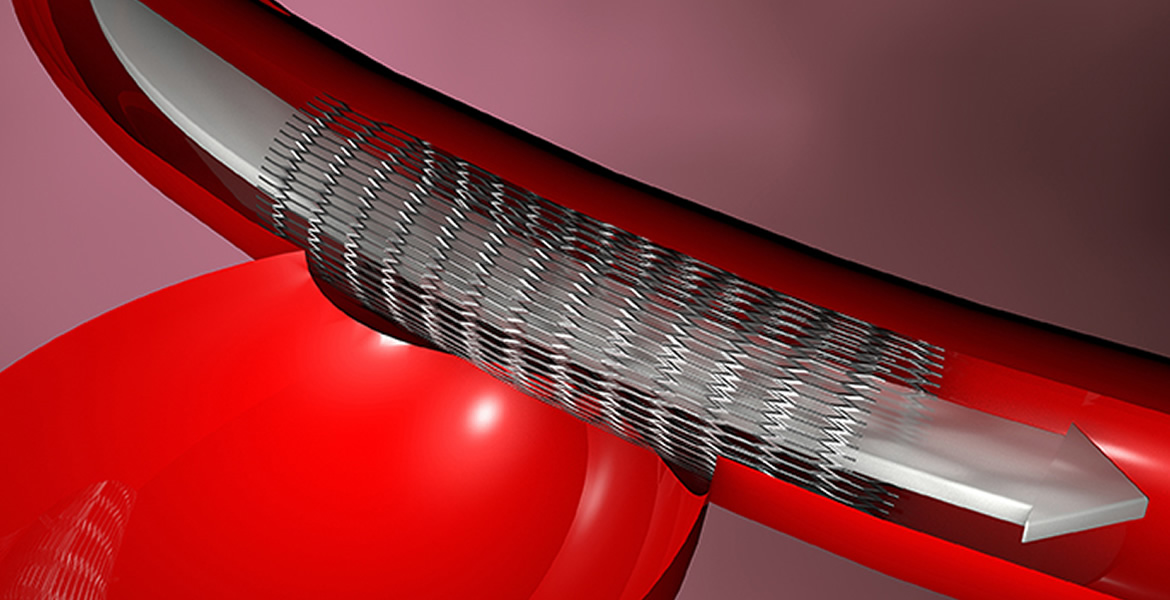
An endovascular stent graft is a tube composed of fabric supported by a metal mesh called a stent. It can be used for a variety of conditions involving the blood vessels, but most commonly is used to reinforce a weak spot in an artery called an aneurysm. Over time, blood pressure and other factors can cause this weak area to bulge like a balloon and it can eventually enlarge and rupture. The stent graft is designed to seal tightly with your artery above and below the aneurysm. The graft is stronger than the weakened artery and it allows your blood to pass through it without pushing on the bulge. Physicians typically use endovascular stent grafting to treat abdominal aortic aneurysms (AAAs), but they also use it to treat thoracic aortic aneurysms (TAAs) and less commonly, aneurysms in other locations.
Aneurysms often affect the aorta, your body’s largest artery. Your aorta carries blood away from the heart and it runs from your heart through your chest and abdomen. The normal diameter of the aorta in the abdomen is about 2 centimeters, which is a little less than 1 inch. An aneurysm is considered to have formed if the aorta grows to more than 1½ to 2 times its normal diameter.
Aortic aneurysms are potentially serious health problems since a burst aorta results in massive internal bleeding that can be fatal unless treated rapidly by an experienced emergency medical team. Endovascular stent graft repair is designed to help prevent an aneurysm from bursting. The term “endovascular” means “inside blood vessels.” To perform endovascular procedures, vascular surgeons use special technologies and instruments. These procedures require only a small incision or puncture in an artery or vein. Through these punctures, a vascular surgeon inserts long thin tubes, called catheters, which carry the devices through your blood vessels to the location of the aneurysm. They can then be placed to re-align and strengthen your artery. Generally, endovascular treatments allow you to leave the hospital sooner and recover more quickly, with less pain and a lower risk of complications, and sometimes a lower risk of death, than traditional surgery because the incisions are smaller. Sometimes traditional surgery is required, however, if the shape or the location of the aneurysm is not favorable for an endovascular treatment. Your vascular surgeon will help you decide what procedure is best for your particular situation.
How do I prepare?
Your physician will ask you about your medical history and perform a complete physical examination. In addition, your physician may perform several tests, including an electrocardiogram (ECG), which measures your heart’s electrical activity, stress testing, which will help to determine your heart health, and a scan to determine if your aneurysm has a favorable shape for endovascular stent graft treatment. If your physician believes that you are a good candidate for endovascular stent grafting, he or she may order one or more of the following tests. These tests show detailed images of your arteries and help your physician choose the correct size and shape of the graft:
- Spiral computed tomography (CT) scan: This test involves a rapid series of x rays taken in a spiral pattern around your body. A computer transforms the x ray data into three-dimensional images of your blood vessels
- Angiography: In these tests, your physician inserts a catheter into one of your arteries. Your physician then injects a dye called contrast through the catheter and takes x rays
Am I eligible for endovascular stent grafting?
You may be eligible for elective (non-emergency) endovascular stent grafting if your aortic aneurysm has not ruptured, is large enough (5 centimeters, about 2 inches, wide or more), and you have a long enough area of normal artery for the stent graft to attach securely. Endovascular stent grafting may be a good option if your risk for conventional surgical aneurysm repair is increased because of other illnesses you might have. However, if you have a long life expectancy or have a low risk for complications, or if the shape of the aneurysm is not favorable for an endovascular stent graft, your physician may recommend conventional surgical aneurysm repair instead. To date, this treatment has been used for a longer period of time than endovascular stent grafting and there is general agreement that it requires less long-term maintenance than endovascular repair.
The physical characteristics of your aneurysm help your physician determine if you are a good candidate for endovascular treatment. For example, if you have an AAA located in the section of the aorta just below your kidney arteries, and there is enough space for the stent graft to seal properly, and your aorta is not severely angled, you may be eligible. Your blood vessels also must be large enough to allow the endovascular stent graft to pass through, and the device must fit the shape and contour of your blood vessels once it is in place.
Stent grafting, as has been stated, is not limited to the aorta. Stent grafting may additionally be an option for aneurysms that occur in arteries in other regions of the body depending on the size and location. Your vascular surgeon will best be able to determine whether your specific aneurysm is amenable to stent graft therapy.
Am I at risk for complications?
If you have kidney disease called chronic renal insufficiency, your chances of complications from endovascular stent grafting may be increased since contrast dye, which can affect the kidneys, is required. If you have an unfavorable aneurysm shape, associated arterial occlusive disease, or have already had an AAA repaired, you also may be at increased risk for complications. Other conditions, such as heart or lung disease, may also increase the risk for treatment. Some of these issues may be addressed by adjunctive measures to lessen the risk of the endovascular procedure if your risk for conventional (open) aneurysm repair is prohibitive. Your vascular surgeon will advise you regarding the best option for your particular situation.
What happens during endovascular stent grafting?
As the procedure begins, you will usually receive a sedative and a regional anesthesia, or you might receive general anesthesia depending upon your particular circumstance. Your vascular surgery team will clean your skin and shave hair around the insertion points to help decrease your chances of infection. Your vascular surgeon will then cut into the skin overlying the femoral artery in your groin. Your vascular surgeon then threads a guide wire into your femoral artery and advances it to the aneurysm. Because you have no nerve endings inside your arteries, you will not feel the wires or catheters as they move through your body. You may feel a slight pressure or a sensation of mild tugging during this insertion.
Using x-rays that appear as moving images on a screen, your vascular surgeon inserts a catheter over the guide wire. Usually your vascular surgeon will perform angiography through the catheter to insure correct placement of the endovascular stent graft. You may feel a warm sensation as the contrast dye is injected. Then, a compressed form of the graft is inserted through a larger catheter, called a sheath, and the guide wire carries so it can move through your blood vessels. When the graft has reached the aneurysm site, your physician withdraws the sheath, leaving the graft in place. The graft expands to fit snugly against the walls of your artery. Often additional components of the graft are placed in a similar fashion through incisions in each groin to extend to the arteries supplying each leg.
What can I expect after endovascular stent grafting?
Usually you will spend 2 to 3 days in the hospital. During the first recovery day you will be permitted to eat and encouraged to walk.
After you leave the hospital, you should not drive until your physician approves. You may be permitted to sponge bathe around your incisions but you should avoid soaking your groin incisions until they have healed. You may also be advised to avoid lifting more than about 5 to 10 pounds for approximately 4 to 6 weeks after the procedure.
Your physician will instruct you to return for a follow-up visit within the first few weeks after your procedure. At that visit, your physician will check your incisions and assess your overall condition.
Usually you will undergo follow-up imaging tests within the first few months after the procedure to ensure that the stent is still functioning without significant problems and in the proper location. After the first year, you will probably undergo yearly imaging tests if your aneurysm is shrinking and no problems are found. You may require more frequent imaging tests if potential problems require closer monitoring.
Are there any complications?
The potential complications of endovascular stent grafting include:
- Leaking of blood around the graft (“endoleaks”)
- Infection
- Movement of the graft away from the desired location (“migration”)
- Graft fracturing
- Blockage of the blood flow through the graft
Sometimes fever and an increase in white blood cell count can happen shortly after endovascular stent grafting. These symptoms usually last 2 to 10 days and are treated with medications such as aspirin and ibuprofen. Other complications that are rare but serious include a burst artery, injury to your kidney, paralysis, blocked blood flow to your abdomen or lower body, and delayed rupture of AAA.
Endovascular stent grafts can sometimes leak blood through the areas where the graft components join together, or they can allow blood to leak back into the aneurysm sac through small arteries feeding the aneurysm sac. These leaks are called “endoleaks,” and while this name is somewhat confusing, it does not imply that your aneurysm has ruptured or is leaking. Some of the leaks stop by themselves and are not dangerous, but others need to be treated immediately. These leaks can even occur years after your procedure and can be dangerous if the aneurysm continues to enlarge. Thus, after endovascular aneurysm repair, physicians require their patients to undergo long term surveillance with periodic CT scans for the rest of their life to detect and treat problems before they become threatening. Since problems with the graft or endoleaks can occur even years after successful placement, it is important to comply with the follow-up regimen advised by your vascular surgeon.
If you suspect or experience any complications because of the endovascular stent graft as described above, you should contact your physician immediately.