Surgical Bypass
What is surgical bypass?
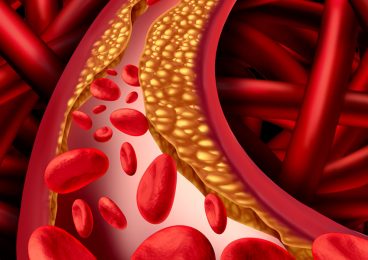
Surgical bypass treats your narrowed arteries by directly creating a detour, or bypass, around a section of the artery that is blocked. Your arteries are normally smooth and unobstructed on the inside but they can become blocked through a process called atherosclerosis, which means hardening of the arteries. As you age, a sticky substance called plaque can build up in the walls of your arteries. Cholesterol, calcium, and fibrous tissue make up the plaque. As more plaque builds up, your arteries can narrow and stiffen. Eventually, as the process progresses, your blood vessels can no longer supply the oxygen demands of your organs or muscles, and symptoms may develop.
During a bypass procedure, your vascular surgeon creates a new pathway for blood flow using a graft. A graft can be a portion of one of your veins or a man-made synthetic tube that your surgeon connects above and below a blockage to allow blood to pass through it and around the blockage.
You may be familiar with bypass surgery on heart arteries, but vascular surgeons also use similar bypasses to treat peripheral arterial disease (PAD). Surgeons use bypasses most commonly to treat leg artery disease, which is hardening of the arteries in the leg. Surgeons also use bypass to treat arm artery disease, as well as blockages involving blood vessels in other locations in the body.
How do I prepare?
First your physician asks you questions about your general health, medical history, and symptoms. In addition, your physician conducts a physical exam and may order a blood test to determine your cholesterol levels. Together, the questions and examination are known as a patient history and exam. Your physician will also want to know when your symptoms occur and how often.
Next, your physician orders tests to locate the blockage and choose the best places to connect the graft. These tests include:
- Duplex ultrasound, which is a non-invasive test that uses high-frequency sound waves to measure real-time blood flow and detect blockages or other abnormalities in the structure of your arteries
- Magnetic resonance angiography (MRA), which uses magnetic fields and radio waves to show blockages inside your arteries
- Computerized tomographic angiography (CTA), which uses contrast dye and x rays (essentially a specialized CT scan), to show blockages inside your arteries
- Angiography, which produces x-ray pictures of the blood vessels in your legs using a contrast dye that is injected to highlight your arteries
If you have arm or leg artery disease, your physician may order segmental blood pressures or pulse volume recording to determine the narrowing of the arteries in your arm or leg. If you have had a heart attack in the past, or if you have chest pain, your physician might recommend a stress test or, possibly, a heart catheterization.
Your physician or vascular surgeon will give you the necessary instructions you need to follow before the surgery, such as fasting. Usually, your physician will ask you not to eat or drink anything 8 hours before your procedure. Your physician will discuss with you whether to reduce or stop any medications that might increase your risk of bleeding or other complications.
Am I a candidate for bypass surgery?
If you have symptoms of atherosclerosis, you may be a candidate for bypass surgery. Symptoms can range from pain in the arms or legs during activity, called intermittent claudication, to the development of non-healing ulcers or gangrene (tissue death) in more severe cases. You still may be a candidate for bypass surgery even if you are not eligible for angioplasty and stenting.
Am I at risk for complications during procedure?
Factors that increase your chances of complications include:
- High blood pressure
- Obesity
- High cholesterol
- Coronary artery disease
- Chronic obstructive pulmonary disease, such as emphysema
- Poor kidney function
- Diabetes
- Smoking
What happens during surgical bypass?
Your specific surgical procedure depends on your symptoms, your overall physical condition, and how much plaque has built up in your arteries. Your surgeon, together with your anesthesiologist, may
recommend either general or regional (epidural or spinal) anesthesia for the procedure.
Although the particular details may vary, in general for an arm or leg bypass, your vascular surgeon usually first selects and removes the vein that will serve as the bypass graft for your artery. Your vascular surgeon usually uses your greater saphenous vein (GSV) for the graft, if it is suitable. Your GSV runs under your skin between your foot and your groin. Sometimes your surgeon may need to use another vein or a synthetic fabric artery for the graft if your GSV is unavailable or unsuitable.
To reach the bypass site in your blocked artery, your surgeon makes an incision in your skin over the artery. Once your surgeon exposes the artery, he or she evaluates the pulse in the healthy part of the artery. By checking the pulse, your surgeon makes sure that the artery provides enough blood flow to supply the bypass.
Your surgeon next opens the artery below the part that is blocked. This is where he or she will connect one end of the graft. Your surgeon sews the graft into your artery with permanent stitches. Next your surgeon routes the other end of the graft between your muscles and tendons to a site above the blockage. The same way, the surgeon then opens the artery and, at this location, stitches the graft onto this end of the artery. Your surgeon checks the bypass for correct alignment and leakage. During the procedure, your vascular surgeon may perform an arteriogram or duplex ultrasound examination in the operating room to check the bypass for any problems. When the surgery is complete, your surgeon closes all of the incisions. After the procedure, your surgeon may order a duplex ultrasound or other non-invasive tests, such as pulse volume recordings, to make sure the bypass is functioning properly.
What can I expect after surgical bypass?
Your hospital stay may range from about 3 to 10 days. Your surgeon will remove staples or stitches from the incisions, usually about 7 to 14 days after your operation, after you leave the hospital. You may need assistance from a visiting nurse, home health aide, or physical therapist when you first go home.
If you develop fevers, a cold painful arm or leg, or if your incision area becomes extremely red, swells, or begins draining, you should contact your physician immediately. These may be signs of developing infection or other problems.
If you have PAD, your physician or surgeon may also recommend that you take an antiplatelet medication, such as aspirin, which can help prevent blood clots.
Are there any complications?
Complications from bypass surgery are possible, but not usual. No procedure is risk-free, but you will experience a minimum number of complications if you select a well-trained vascular surgeon who specializes in the type of bypass surgery that your symptoms indicate. Some complications from bypass surgery are less serious and may include swelling or inflammation at the incision site. Others, such as blockage of the bypass, bleeding from the incision or infection, are potentially more serious. Your vascular surgeon will discuss the important risks and benefits with you and answer your particular questions.
What can I do to stay healthy?
Surgical bypass does not stop plaque build up. If you have bypass surgery, you should make changes in your lifestyle to preserve the success of your bypass graft. You should seriously consider changes that will help lower your blood pressure and decrease the chances that plaque will affect your graft or other arteries. These changes include:
- Eating foods low in fat, cholesterol, and calories
- Controlling blood cholesterol and lipid (fat) levels
- Maintaining your ideal body weight
- Exercising aerobically, such as brisk walking, for 20 to 30 minutes at least 5 times each week
- Quitting smoking